What Will It Take to End TB?
Tuberculosis (TB) continues to be a leading cause of death worldwide, with a disproportionate impact on the global south. The infectious bacterial disease is not only treatable but also curable and preventable: an estimated 54 million lives were saved through TB diagnosis and treatment between 2000 and 2017.
Each year, World TB Day is recognized on March 24th to raise awareness about the disease, its impact on communities across the globe and efforts to eliminate it. The theme this year is It’s Time—to test and treat latent TB infection; to strengthen TB education and awareness among healthcare providers; to speak up; to end stigma; and to end TB.
To learn about what it will take to end TB, we talked to our Director of Pediatric Nursing, and former Seed Nurse Educator, Dr. Brittney van de Water, who is currently a postdoctoral fellow at Harvard Medical School, Department of Global Health and Social Medicine. Brittney’s current research focuses on examining appropriate treatment for individuals with drug-resistant tuberculosis and HIV in South Africa and Peru.
What drew you to study TB?
I became interested in TB while studying abroad in South Africa at Rhodes University in 2008. I volunteered at a local hospital and knew the HIV epidemic was terrible in South Africa, but at the time, I didn’t know much about TB. While volunteering on the pediatric unit, there were quite a few children sick with TB. Then, while working as a nurse educator in Malawi, I was shocked to see so many pediatric patients with TB too. While looking at PhD programs, one mentor was focusing on drug-resistant TB in South Africa, so I jumped at the opportunity to study TB in a high HIV prevalence setting. Since then, I have continued to learn about TB and now focus on TB household contact management interventions so that we can prevent TB in high-risk individuals (such as household contacts) in addition to treating TB.
What are the best strategies for eliminating TB?
I am not sure there is ONE best strategy to eliminate TB. I think we (researchers, clinicians, policy makers, and community members) have to work together to comprehensively (and rapidly!) eliminate TB. The project I’m working on is trying to systematically search for new cases of TB, support individuals on TB treatment, and prevent TB through active household contact management. Instead of placing the burden on patients and their family members, we as healthcare providers must go and visit patients in their homes. Providing education and empowerment to communities, so that they know the signs and symptoms of TB, and making TB diagnosis and care more accessible can also help in the fight against it.
What are some of the leading barriers to identifying and treating TB?
There are many barriers to identifying and treating TB, especially in low-resource settings, such as sub-Saharan Africa. For patients, the barriers are limited knowledge, attitudes and beliefs regarding TB, and economic burdens which limit TB identification and treatment. From a health systems perspective, barriers include centralization of services, health system delays, and limited geographical access to healthcare. Additionally, diagnosing TB in children can be especially difficult; yet, if treated, children often have very good clinical outcomes.
Your research speaks to the importance of recommended care guidelines for clinical providers, how does education and training help to improve awareness of and adherence to such guidelines?
Part of my dissertation focused on concordance between national guidelines and provider prescriptive practices for patients with drug-resistant TB. We found that most patients received the correct medications, yet few patients were prescribed the right medications, at the right dosage, and at the right frequency (i.e. number of times medicine was prescribed per week). This is concerning because most patients were under-dosed, which could lead to more drug resistance developing.
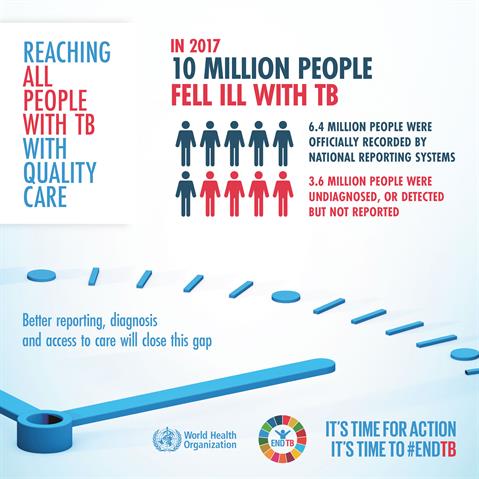
I believe all clinicians do their best to provide care to their patients. Having health systems that support clinicians is important. For example, if guidelines are weight based, there must be scales available so that patients can be weighed accurately. Providing appropriate training when new guidelines are published is also important. Health systems must empower providers to give the best care possible and health systems must empower patients with access to the healthcare they deserve. The leading cause of death from an infectious disease globally is TB, killing more people each year than HIV, yet few people in developed countries are aware that TB is such an enormous global issue.
The work done by researchers like Brittney will help guide the training and education of clinicians, and increase the capacity for quality TB treatment, care, and prevention.

